Acupuncture and herbs improve eyesight for patients with diabetic retinopathy. In a controlled clinical trial, Hubei Provincial Hospital of Traditional Chinese Medicine ophthalmology department researchers determined that herbal medicine monotherapy benefits vision. The addition of acupuncture to the treatment protocol significantly improved patient outcomes.
Diabetic retinopathy patients receiving acupuncture and herbal medicine demonstrated significant improvements in visual acuity. Also, patients demonstrated improvements in the health of the retina; there were reductions in ocular microaneurysms, hard exudate, cotton wool spots, retinal bleeding, edema, and leaking blood vessels. [1]
Before and after treatment, the data was verified with visual acuity tests (with the naked eye and correctional lenses). Additional tests confirm the data, including intraocular pressure and slit lamp exams. Testing of ocular blood flow, retinal thickness, and other parameters were tested with fluorescein angiography (FFA) and optical coherence tomography (OCT). OCT employs the use of light waves to take images of tissues that receive light. Glycated hemoglobin (HbA1c) and blood glucose levels were also taken into account.
The severity of diabetic retinopathy was assessed by the presence of various ocular clinical signs including: microaneurysms, hard exudate, cotton wool spots, retinal bleeding, edema, and the formation of new blood vessels. Patients showing improvement in four or more of these six areas were was classed as markedly effective. Patients showing improvement in two or more areas were classed as effective. Patients with no change were classified as ineffective. In the herb monotherapy group, 10 patients were markedly effective and 15 effective, producing a total effective rate of 71.4%. In the acupuncture plus herbs group, 15 patients were markedly effective and 15 were effective, producing a total effective rate of 83.3%. Visual acuity improved in both study groups: 58/70 in the herb monotherapy group and 61/72 eyes in the acupuncture plus herbs group.
Traditional Chinese Medicine
According to Traditional Chinese medicine (TCM) principles, diabetes mellitus is caused by qi and yin deficiency, stemming from liver and kidney deficiency syndrome. This leads to interior heat and dryness, bodily fluid and endogenous secretion insufficiency, and the formation of phlegm. These differential diagnostic imbalances result in blood stasis and reduced ocular blood flow. Primary treatment principles include supplementing qi, nourishing yin, and resolving blood stasis. On this basis, the participants in both groups were prescribed He Xue Ming Mu tablets, which contain the following ingredients:
- Sheng Pu Huang
- Sheng Di Huang
- Huang Qin
- Han Lian Cao
- Dan Shen
- Yu Jin
- Chuan Xiong
- Mu Dan Pi
- Chi Shao
- Ju Hua
- Xia Ku Cao
- Chong Wei Zi
- Nu Zhen Zi
- Jue Ming Zi
- Che Qian Zi
A dose of five tablets (1.5g) was taken three times daily, swallowed with warm water after meals. Each course of treatment lasted 15 days and was separated by a three day interval. Follow-up appointments were administered two months into the treatment period and again after six months.
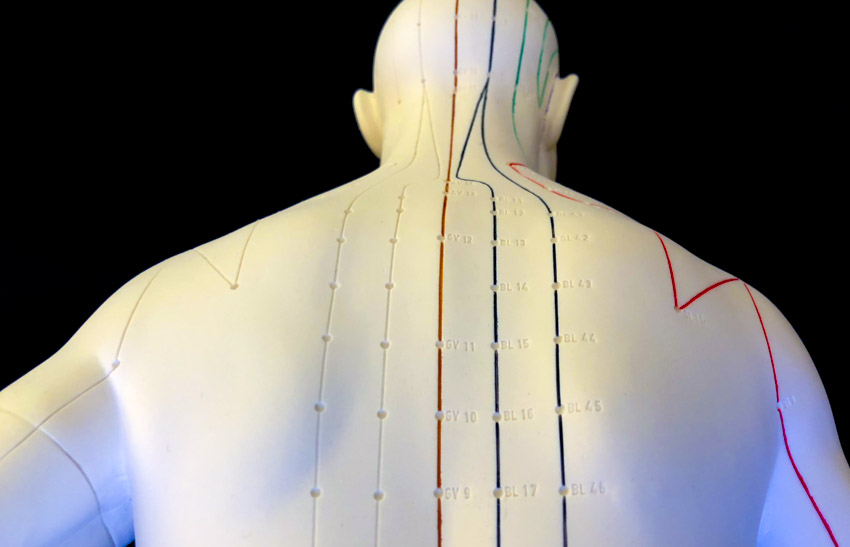
Acupuncture Treatment
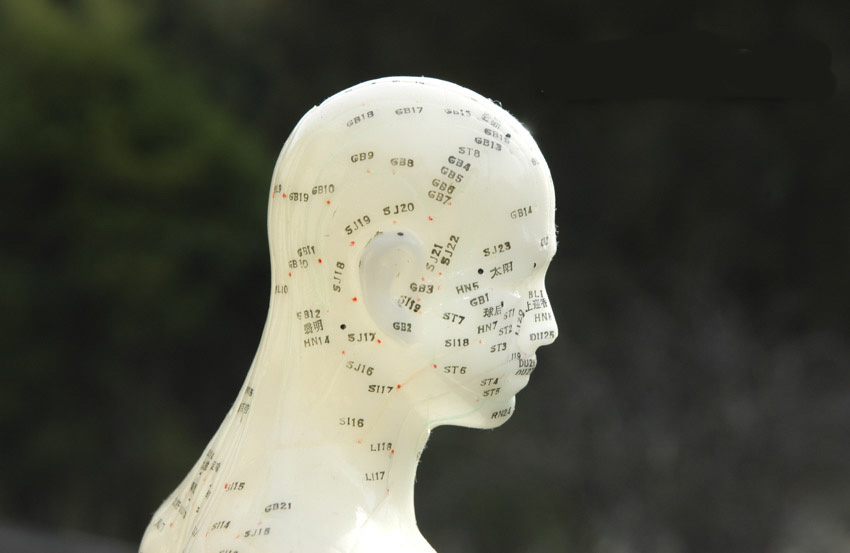
In addition to He Xue Ming Mu tablets, participants in the acupuncture plus herbs group received acupuncture treatments. Treatment began with patients in a seated position and, following standard disinfection, 0.35mm × 40mm filiform needles were inserted at the following primary acupoints:
- Fengchi (GB20)
- Jingming (BL1)
- Taiyang (MHN9)
- Zanzhu (BL2)
- Sizhukong (TB23)
Needles were inserted slowly and were manipulated using a balanced reinforcing-reducing technique, with a suitable degree of needle sensation directed towards the eyes. After obtaining deqi, needles were retained for 30 minutes. The patients were then moved to a treatment couch, and needles were inserted into the following secondary acupoints:
- Guanyuan (CV4)
- Sanyinjiao (SP6)
- Ganshu (BL18)
- Shenshu (BL23)
Needles were manipulated using a reinforcing method and were retained for 30 minutes. Treatments were administered every two days, with 30 days making up one course of care. A total of two courses were administered. The results indicate that herb monotherapy and acupuncture plus herbal medicine are both effective treatments for diabetic neuropathy.
Vision Loss
Diabetic retinopathy is the number one cause of vision loss. Diabetes affects more than 280 million people worldwide and about one third suffer from diabetic retinopathy. [2] Risk factors for diabetic retinopathy include hyperglycemia and hypertension. Diabetic retinopathy has been “ranked as the fifth most common cause of preventable blindness and fifth most common cause of moderate to severe visual impairment.” [3] The National Institutes of Health notes, “Diabetic retinopathy affects blood vessels in the light-sensitive tissue called the retina that lines the back of the eye. It is the most common cause of vision loss among people with diabetes and the leading cause of vision impairment and blindness among working-age adults.” [4]
All patients with diabetes are at risk. Early symptoms of diabetic retinopathy include a decrease in color vision, blurry vision, floaters or spots, dark areas in the visual field, and vision loss. Over time, the high blood sugar levels in diabetics may damage blood vessels in the retina (the eyeball rear layer containing light sensitive cells that send nerve impulses to the optic nerve). This causes fluid or blood leakage, which distorts vision. This may lead to scarring and retinal cell loss.
Outcomes
The outcomes of this study indicate that acupuncture combined with He Xue Ming Mu tablets improves visual acuity and slows the progression of diabetic retinopathy. To learn more, contact a local licensed acupuncturist.
The use of herbal medicine and acupuncture for the treatment of eye disorders has a long history in Traditional Chinese Medicine (TCM). One classic herbal formula used for the treatment of diabetic retinopathy and wet macular degeneration is Ning Xue Tang, containing the following ingredients:
- Xian He Cao
- Ce Bai Ye
- Han Lian Cao
- E Jiao
- Sheng Di Huang
- Bai Mao Gen
- Zhi Zi Tan
- Bai Shao
- Bai Ji
- Bai Lian
The clinical trial tested He Xue Ming Mu tablets, which shares Sheng Di Huang with Ning Xue Tang. Chi Shao is used in place of Bai Shao in Ning Xue Tang, focusing on invigorating and cooling blood over tonifying blood. Otherwise, this classic formula greatly varies from He Xue Ming Mu tablets. This, in part, is due to the fact that TCM has many individual herbs and herbal formulas that are designed for benefitting the eyes across multiple diagnostic patterns. Given the importance of eyesight, additional research is warranted to investigate the efficacy of acupuncture and herbal medicine for the treatment of vision disorders.
References:
1. Zhu Dan (2018) “Clinical Observation on Acupuncture Combined with He Xue Ming Mu Tablets in Treatment of Diabetic Retinopathy” Journal of Hubei University of Chinese Medicine Vol. 20 (4), pp. 87-89.
2. Lee, Ryan, Tien Y. Wong, and Charumathi Sabanayagam. “Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss.” Eye and vision 2, no. 1 (2015): 17.
3. Ibid.
4. nei.nih.gov/health/diabetic/retinopathy