Acupuncture promotes the healing of bone fractures. Two independent investigations confirm that the addition of acupuncture to usual care protocols increases positive patient outcomes rates. Researchers find acupuncture effective for assisting in the restoration of mobility and reductions in both pain and inflammation.
The first investigation was conducted at The People’s Hospital of Hengfeng County. All patients had severe tibiofibular fractures (lower leg). All received surgical correction, requiring insertion of metal rods into the bone (internal fixation with intramedullary nails). The second investigation was conducted at The Traditional Chinese Medicine Hospital of Anyi County. All patients had supracondylar fractures of the humerus (upper arm near the elbow), a type of fracture common in children and teenagers. For both the arm and leg fractures, acupuncture significantly reduced swelling and pain. In addition, acupuncture resulted in improved functioning at the injured sites, with significant improvements in range of motion. [1], [2]
The first study was designed to investigate the effects of acupuncture on patients with tibiofibular fractures that underwent internal fixation procedures with interlocking, intramedullary nails. In this procedure, a long, metal rod is inserted into the bone and held in place with screws at either end. It is most commonly used in fractures of the long bones and prevents the bone from moving as it heals.
A total of 94 patients were recruited for the study and were randomized to either an acupuncture group or a control group. The acupuncture group consisted of 47 participants, aged 21–56 years (mean age 37.9 years). Of these patients, 25 had open fractures and 22 had closed fractures. The control group consisted of 47 participants, aged 22–58 years (mean age 38.1 years). All participants had the exact type, location, and direction of their fractures confirmed by X-ray imaging. Inclusion criteria for the study were the following: fracture type suitable for surgery, no obvious contraindications for surgery. Exclusion criteria were the following: pre-existing heart, liver, kidney, or cerebral disease.
The two groups were statistically similar in terms of baseline characteristics. Both groups were given internal fixation surgery with interlocking intramedullary nails. From the second postoperative day, they were prescribed functional rehabilitation exercises. Participants in the acupuncture group received acupuncture, while participants in the control group were treated with the herbal medicine Jie Gu Qi Li Pian (bone setting pills). The pills contain the following herbs: Ru Xiang, Mo Yao, Dang Gui, Di Bie Chong, Gu Sui Bu, Peng Sha, Long Xue Jie, Zi Ran Tong, and Da Huang. They are indicated for promoting circulation and preventing blood stasis. A 1.5g dose was given twice daily, for a total of 60 days.
Acupuncture Procedure
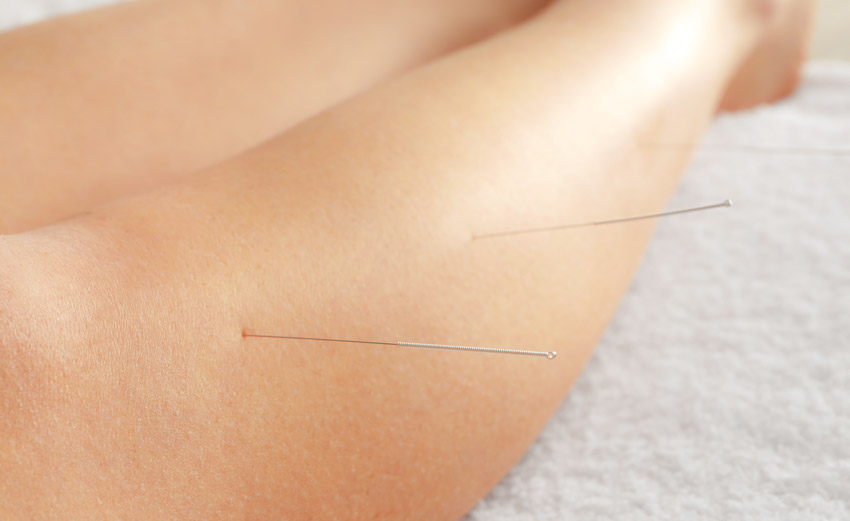
Acupuncture treatments were administered with patients resting on a treatment couch, with their affected leg in a raised position. The following acupoints were selected:
- Baihui (GV20)
- Shenshu (BL23)
- Zusanli (ST36)
- Neiguan (PC6)
- Dazhu (BL11)
- Geshu (BL17)
In addition, the following acupoints were only applied to the affected side:
- Taichong (LV3)
- Fenglong (ST40)
- Xuehai (SP10)
- Yanglingquan (GB34)
- Ashi points
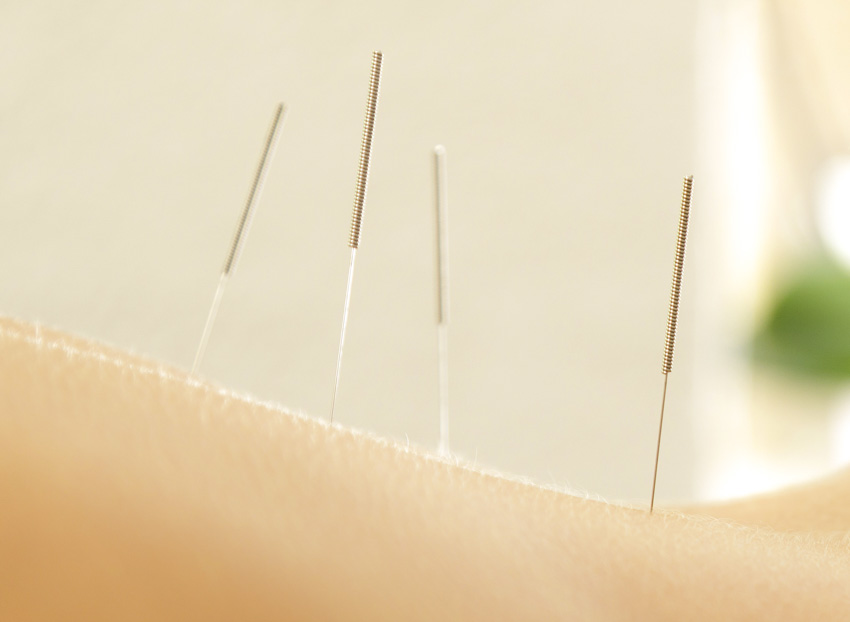
Needles were inserted into each acupoint and were stimulated with moderate strength. All points were stimulated using a reinforcing technique, with the exception of Fenglong (ST40), which was stimulated using a balanced reinforcing-reducing technique. All needles were retained for 30 minutes. Treatments were administered daily, with seven days making up one course of care. A total of two courses were provided, separated by a three day interval.
Outcomes
All participants were re-examined 60 days after surgery and their fractures were classified as healed, partially healed, or unhealed. Participants classified as healed showed no abnormal range of motion, no tenderness or longitudinal pain, and X-rays confirmed the complete healing of the fracture. Participants classified as partially healed showed no abnormal range of motion, some residual tenderness or longitudinal pain, and X-rays showed partial healing of the fracture. Participants classified as unhealed showed abnormal range of motion, residual tenderness or longitudinal pain, and X-rays confirmed that the fracture remained in poor condition. Swelling of the affected limb was also measured before and seven days after surgery by measuring the circumference of the leg. This compared with the healthy leg, and the degree of swelling was quantified as a percentage.
In the control group, 22 participants were classified as fully healed, 16 were partially healed, and 9 were unhealed. The total effective rate was 80.9%. In the acupuncture group, 32 participants were classified as fully healed, 13 were partially healed, and 2 were unhealed. The total effective rate was 95.7%. The results demonstrate that significantly greater improvements were experienced by participants in the acupuncture group. In addition, greater reductions of swelling were in the acupuncture group, falling from a mean 8.45% before surgery to 4.51% after seven days. This is compared with a reduction from a mean 8.52% to 7.02% in the control group. Based on the results, it was calculated that swelling subsided in 9.46 days for patients in the acupuncture group, compared with 14.93 days for the control group patients.
Humerus
The second study examined acupuncture treatments for supracondylar fractures of the humerus. A total of 64 patients were recruited for the study and were randomly assigned to the acupuncture group or the control group. The acupuncture group consisted of 32 participants, aged 6–14 years (mean age 8.17) and the control group consisted of 32 participants, aged 5–14 years (mean age 8.23). All participants were diagnosed with unilateral supracondylar fractures of the humerus. The fractures were due to a combination of traffic accidents, falls, or other injuries.
Inclusion criteria for the study were the following: diagnosis of a supracondylar fracture confirmed by X-rays, age 5–14 years, fractures with a Gartland classification of III (complete displacement), and fractures less than one week old. Exclusion criteria were the following: open fractures, nerve or blood vessel damage, and concurrent heart, liver, kidney or nervous system disease. The two groups were statistically similar in terms of baseline characteristics prior to the investigation.
Both groups were given standard treatments for fractures including surgery or manipulations to reposition the bones. Support with a splint or plaster cast was provided. Patients were prescribed Xue Sai Tong intravenous fluid, a preparation primarily made up of San Qi, an herb used to arrest bleeding and resolve blood stasis. This was administered daily for 14 days, with 0.2g given each time.
Acupuncture Procedure
The following acupoints were selected for the study:
- Dazhu (BL11)
- Geshu (BL17)
- Shenshu (BL23)
- Zusanli (ST36)
- Ashi points
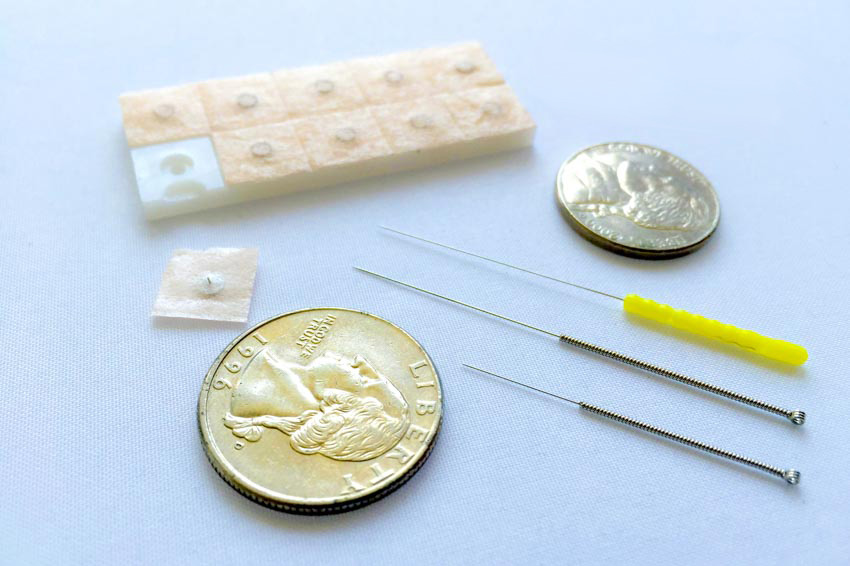
Following standard disinfection, 0.25 × 25mm single-use needles were used to needle the acupoints. After obtaining deqi, the needles were stimulated using moderate strength and were retained for 30 minutes. Treatment was administered daily for a total of 14 days.
Outcomes
Outcomes were assessed after 12 months using the Neer classification for humeral fractures. Patients received a score out of 100 divided into 35 points for pain, 30 for shoulder function, 25 for range of motion, and 10 for anatomical location. Participants in the acupuncture group scored consistently higher across all areas with a total score of 88.2, compared with 80.09 in the control group.
The efficacy of the treatment was also classified as either excellent, good, satisfactory, or unsatisfactory based on the participants’ clinical characteristics following the study. Those classified as excellent had normal range of motion in the elbow, those classified as good had their range of motion affected by 10 degrees or less, those classified as satisfactory had their range of motion affected by 10–20 degrees, and those classified as unsatisfactory had their range of motion affected by 20 degrees or more.
In the control group, 9 participants were classified as excellent, 16 as good, 5 as satisfactory, and 2 as unsatisfactory. In the acupuncture group, 18 participants were in the excellent category, 11 were classified as good, 2 as satisfactory, and just 1 as unsatisfactory. The excellent and good scores were added together to give the total effective rate, which was significantly higher in the acupuncture group at 90.62% compared with 78.13% in the control group.
The results of the aforementioned studies indicate that acupuncture significantly improves outcomes for patients with bone fractures. Acupuncture promotes a more complete healing of the bones, improves range of motion, and facilitates faster reductions in swelling and pain. To learn more, contact a local licensed acupuncturist.
References:
[1] Peng Zhen, Jiang Zelong, Teng Ning (2018) “Effect of Acupuncture on Rehabilitation of patients with Tibiofibular Fracture Undergoing Internal Fixation.” Chinese Journal of integrative Medicine Vol. 22 (26), pp. 3717-3718.
[2] Liu Guanglin, Fu Jingdong, Wang Yan (2018) “Clinical Role of Acupuncture Combined with Xuesaitong in the Treatment of Supracondylar Fracture of the Humerus.” Chinese Journal of integrative Medicine Vol. 22 (26), pp. 3719-3720.