Dalian Hospital of Traditional Chinese Medicine researchers confirm that acupuncture combined with herbal medicine is effective for the treatment of insomnia in Parkinson’s disease patients. In a controlled clinical trial, a combination of scalp acupuncture and a modified version of the herbal formula Gui Pi Tang were tested. Using the Pittsburgh Sleep Quality Index (PSQI) as a quantitative measure, Parkinson’s disease patients demonstrated significant improvements in sleep. [1]
The PSQI scale rates subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction. Higher numbers indicate worse overall quality of sleep. PSQI questionnaires completed before and after the treatment period showed a statistically significant improvement in sleep quality in the two Chinese medicine groups. Group one received acupuncture and herbal medicine and group two received only herbal medicine.
Participants in the acupuncture plus herbs group showed a greater improvement in sleep quality with PSQI scores reduced from a mean of 14.9 before treatment to 4.5 following treatment. Improvements in the herbal medicine monotherapy group were comparatively lower, reducing from a mean of 15.1 to 8.7 following treatment. The results indicate that although herbal medicine is effective, the addition of acupuncture to the treatment protocol significantly increases positive patient outcomes for Parkinson’s disease patients suffering from insomnia.
Insomnia is a common Parkinson’s disease complication, with between 70% and 95% of Parkinson’s sufferers affected. Symptoms such as tremors, stiffness, pain, and restless leg syndrome all make getting a good night’s sleep difficult. Also, common Parkinson’s disease medications (e.g., levodopa) have a stimulatory effect and can cause sleep problems if taken late in the evening.
A total of 50 patients with Parkinson’s disease were recruited for the study and were randomized to either the herb monotherapy group (n=25) or the acupuncture plus herbs group (n=25). The herb monotherapy group received a modified Gui Pi Tang formula, while the acupuncture plus herbs group received the identical modified Gui Pi Tang herbal formula plus scalp acupuncture points. Both groups were statistically similar in terms of demographics, with 13 males and 12 females in each group. The mean age of the herb monotherapy group was 69.7 years and the mean age of the acupuncture plus herbs group was 69.6 years.
Inclusion criteria for the study included tremors or mobility problems, stiffness of the limbs affecting the gait, and having undergone an MRI scan to rule out cerebral bleeding. According to Chinese medicine principles, the patients were diagnosed with a pattern of heart and spleen deficiency. This pattern is a combination of heart qi and blood deficiency with spleen qi deficiency. Common indications for the presence of this pattern are insomnia, forgetfulness, palpitations, dream disturbed sleep, poor appetite, and loose stools. The tongue is typically pale with a white coating and the pulse is deep and weak.
For heart and spleen deficiency, the treatment principle is to tonify the heart and spleen. The diagnostic inclusion parameter of heart and spleen deficiency matches the classical application of Gui Pi Tang within Traditional Chinese Medicine (TCM) for the treatment of this condition. In many clinical scenarios, Gui Pi Tang is used for patients that are light sleepers and wake frequently throughout the night. This is distinguished from other forms of sleep disorders. For example, if patients wake between 1–3 am and have stress, anxiety, tight jaws or grinding, and other manifestations of liver qi stagnation, an herbal formula such as Xiao Yao Wan or Dan Zhi Xiao Yao Wan are usually prescribed instead.
Exclusion criteria included reduced liver and kidney function, gastrointestinal bleeding, organ failure, abnormal cerebral function, stroke or cerebral bleeding, and psychological diseases. All of the participants were on various medications including antibiotics, blood pressure medications, or blood sugar regulatory drugs. All participants were prescribed oral levodopa (0.25mg, three times per day). The modified Gui Pi Tang formula consisted of the following herbs:
- Bai Zhu 15g
- Ren Shen 10g
- Dang Gui 15g
- Fu Ling 15g
- Yuan Zhi 10g
- Suan Zao Ren 15g
- Mu Xiang 10g
- Long Yan Rou 10g
- Da Zao 10g
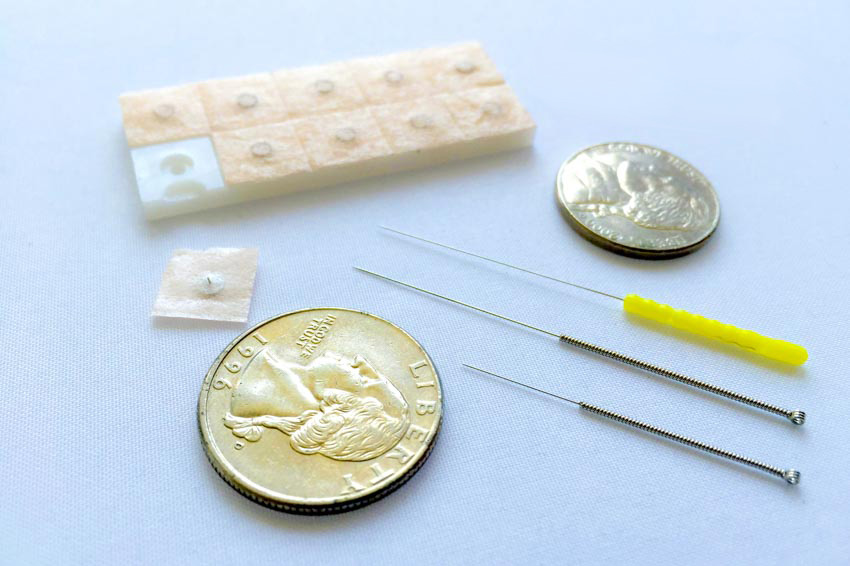
These ingredients were decocted to 150ml of liquid to be taken orally twice per day. Each course lasted 15 days and a total of four courses were administered to both the herb monotherapy and the experimental groups. In addition to the modified Gui Pi Tang formula, the acupuncture plus herbs group also had scalp acupuncture treatments. The following points were selected for all participants:
- Baihui (GV20)
- Touwei (ST8)
- Sishencong (MHN1)
- Toulinqi (GB15)
The acupoints were stimulated manually using a reinforcing method and treatment was administered once per day. Each acupuncture course lasted 15 days (one treatment session per day) and a total of four courses were administered. The results demonstrate significant improvements from the herb monotherapy; however, the addition of acupuncture produces greater clinical results.
Related Research
Federal University of Pernambuco (Recife, Brazil) researchers had similar findings. In this study, 22 patients diagnosed with Parkinson’s disease by a neurologist were recruited and randomized to receive either acupuncture (n=11) or no intervention (n=11). Both groups included seven male and four female participants. The mean age in the acupuncture group was 65 years compared with 56 years in the control group. Despite this difference in age, both groups had similar clinical characteristics.
Inclusion criteria included a diagnosis of idiopathic Parkinson’s disease according to the UK Parkinson’s Disease Society Brain Bank criteria, stage I–III Parkinson’s disease according to the Hoehn-Yahr scale, and ages ranging between 35–80 years. Exclusion criteria included the presence of comorbid neurological diseases, cognitive impairment, or having undergone physiotherapy. All participants had been on a stable dose of Parkinson’s medications for at least 2 months prior to the study. The following acupuncture points were selected for the study on the basis of previous research:
- Taichong (LV3)
- Sanyinjiao (SP6)
- Hegu (LI4)
- Waiguan (TB5)
- Shenmen (HT7)
- Neiguan (PC6)
- Quchi (LI11)
- Fengchi (GB20)
Needles were retained for 30 minutes per session and treatments were administered weekly for a total of eight weeks. The results were analyzed using the Parkinson’s Disease Sleep Scale (PDSS), a self-administered scale which comprises 15 items including overall quality of sleep, sleep onset and maintenance, nocturnal restlessness, nocturnal psychosis, nocturia (excessive waking for urination at night), nocturnal motor symptoms, sleep refreshment, and daytime dozing. There were no significant differences in PDSS scores between the groups prior to the study.
Following treatment, there was a significant improvement in PDSS scores in the acupuncture group in the domains of general sleep quality, nocturnal psychosis, and nocturnal motor symptoms. [2] There was a tendency towards improvement in sleep onset and maintenance, nocturnal agitation, nocturia, relaxing sleep, and daytime sleepiness, but these improvements were not as pronounced as the aforementioned improvements. The control group did not show significant improvements at the end of the study period. Based on the data, the researchers confirm that acupuncture improves sleep for patients with Parkinson’s disease.
References:
1. Li L. “Clinical Observation on Guipi Decoction Combined with Acupuncture and Moxibustion in the Treatment of Insomnia Patients with Parkinson” Guangming Journal of Chinese Medicine; July 2018. Vol 33.
2. De Amorim Aroxa, Fábio Henrique, Ihana Thaís Guerra de Oliveira Gondim, Elba Lúcia Wanderley Santos, Maria das Graças Wanderley de Sales, Amdore Guescel C. Asano, and Nadja Maria Jorge Asano. “Acupuncture as Adjuvant Therapy for Sleep Disorders in Parkinson’s Disease.” Journal of acupuncture and meridian studies 10, no. 1 (2017): 33-38.