Acupuncture is an effective treatment modality for the alleviation of fibromyalgia. Researchers at the Physical Medicine and Rehabilitation Department of Ataturk University conclude that acupuncture improves two biochemical markers and clinical outcomes for patients with fibromyalgia. Objective measures show that acupuncture increases serum serotonin levels while simultaneously reducing Substance P levels. For subjectives, the researchers document lasting subjective improvements including less pain, fatigue, and anxiety. [i]
Fibromyalgia is a chronic condition with a variety of symptoms including widespread pain, sleep problems, fatigue, and cognitive difficulties. Fibromyalgia is frequently comorbid with depression and anxiety. The exact mechanism of the disease is has not been fully identified within allopathic and hospital medicine, but it is thought that serotonin and Substance P play an important role.
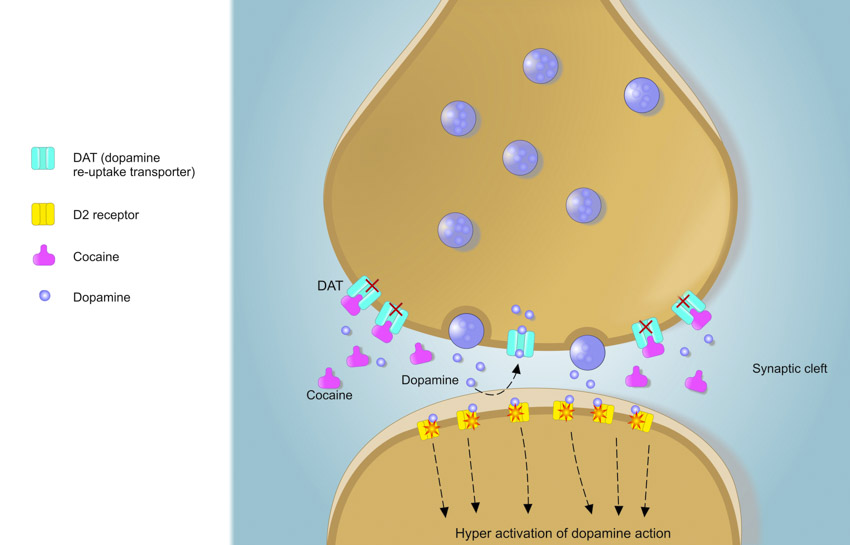
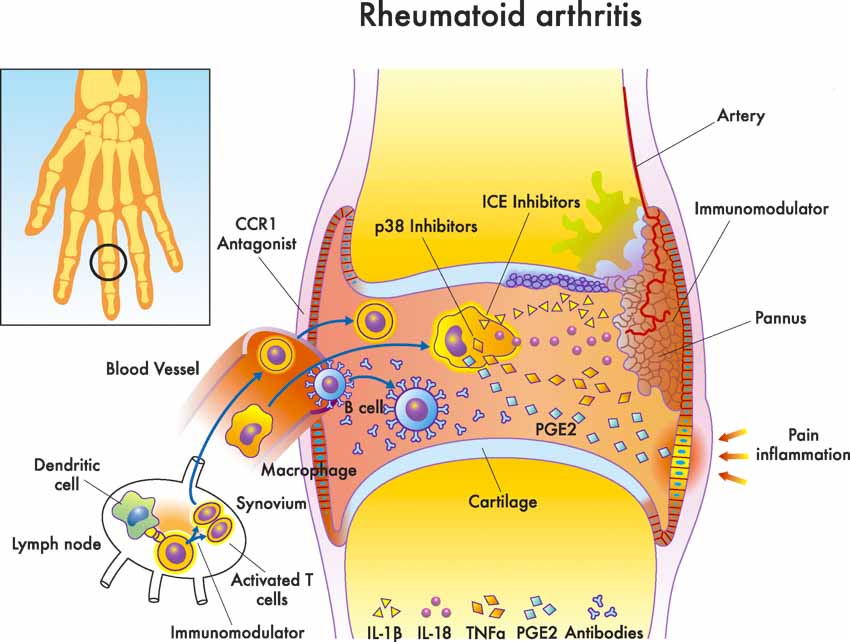
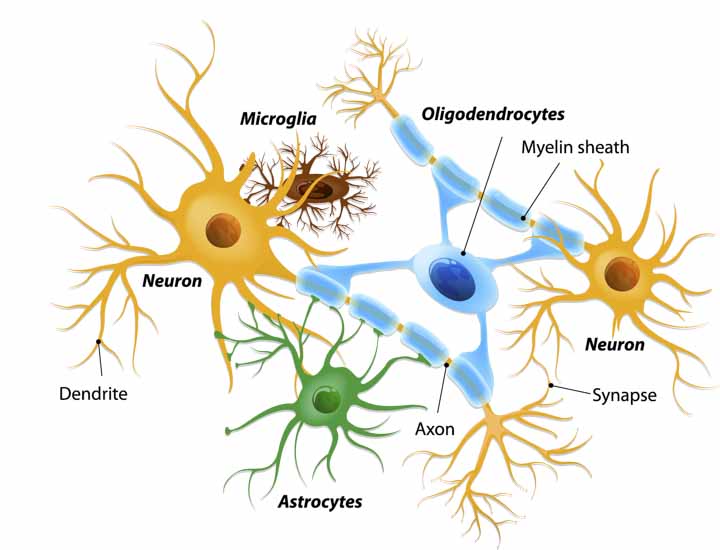
Serotonin is a neurotransmitter involved with mood, sleep, sexual behaviour, and pain regulation. Independent research confirms that fibromyalgia patients have lower serum serotonin levels compared with healthy individuals. Substance P is a neuropeptide involved in pain sensitivity, depression, and peripheral neurogenic inflammation. [ii] Excess levels of Substance P may play a role in the pathology of fibromyalgia, especially since Substance P has an active role in pain perception.
The study measures levels of these two biochemical markers along with several clinical parameters, both before and after treatment with acupuncture. A total of 75 female participants were recruited for the study. Exclusion criteria included usage of non-steroidal anti-inflammatory drugs, selective serotonin reuptake inhibitors, tricyclic antidepressants, and other antidepressant drugs within the past 15 days. Those who had smoked tobacco, suffered from bleeding diathesis, or had painful conditions other than fibromyalgia were also excluded.
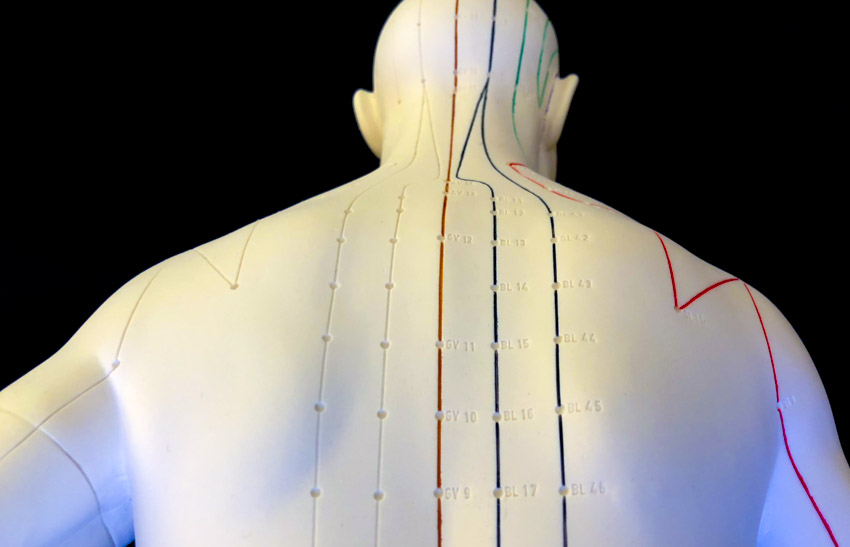
The patients were randomized into three groups; acupuncture, sham acupuncture, and simulated acupuncture. All three groups were similar in terms of mean age and body mass index. The mean duration of disease was 4.44 years, 3.94 years, and 5.09 years respectively. The following acupuncture points were selected for the study:
- Dazhui (GV14)
- Jianzhongshu (SI15)
- Hegu (LI4)
- Quchi (LI11)
- Shenmen (HT7)
- Neiguan (PC6)
- Qihai (CV6)
- Taichong (LV3)
- Zusanli (ST36)
- Sanyinjiao (SP6)
The points were needled bilaterally using 0.25 × 25mm sterile stainless steel filiform acupuncture needles. The needles were retained for 30 minutes per acupuncture session, without manual manipulation during needle retention.
The sham acupuncture group was included to act as a control and to identify the physiological effects of inserting needles into the skin at non-acupuncture points. Sham points were selected within an approximate 1–2cm radius of the true acupoints used in the acupuncture study group. These were identified using an electronic acupuncture point detector to find areas with a weaker signal compared with the genuine acupuncture points.
The simulated acupuncture group was included as a control and to identify the psychological effects of acupuncture treatment. Small, round adhesive bandages were applied to the same points as those used in the acupuncture group. Small needles (0.25 × 15mm) were inserted shallowly into the bandages, but were not allowed to penetrate the skin.
The three groups were blinded using a three section folding hospital screen with the bottom of one of the sections detached allowing the screen to be rolled up. A treatment couch was pushed into this space, and with the patient in position, the screen was dropped over the neck area to block their view. The needles at Dazhui and Jianzhongshu were inserted first, with patients in a seated position. Patients were then asked to recline in a supine position, safely resting in the space between the foldable head and body sections of the couch while the remaining needles were inserted. For all three groups, treatment was administered twice weekly for a total of four weeks.
Results
Serum serotonin and Substance P levels were monitored before and after treatments using a commercial enzyme immunoassay kit, along with several other clinical parameters. A Visual Analogue Scale (VAS) was used to measure widespread pain. The Fibromyalgia Impact Questionnaire (FIQ) was used to measure work status, depression, anxiety, morning tiredness, pain, stiffness, fatigue, and well-being. The Nottingham Health Profile (NHP) was used to measure quality of life including pain, energy, physical mobility, emotional reactions, social isolation, and sleep. Finally, the Beck Depression Inventory (BDI) was used to measure a total of 21 different items including mood, social withdrawal, insomnia, and fatigue. The number of tender points (NTP) for each patient was also taken into account. All parameters were measured at baseline and after treatment. Follow-up visits were performed one month and three months after completion of treatment.
Patients in the acupuncture group experienced significant improvements in VAS (p<0.001), FIQ (p<0.001), BDI (p<0.001), NTP (p<0.001), and some aspects of NHP following treatment. Most of these improvements continued at the three month follow-up. Patients in the sham acupuncture group experienced significant improvements in VAS (p<0.01), FIQ (p<0.05), BDI (p<0.01), and NTP (p=0.001) following treatment. However, only the improvements in FIQ and NTP continued at the three month follow-up. Patients in the simulated acupuncture group experienced significant improvements in VAS (p=0.001), BDI (p<0.01), and NTP (p=0.01), but these improvements discontinued by the three month follow-up.
These findings indicate that sham acupuncture and simulated acupuncture provide a short-term placebo effect but do not provide long-term results. True acupuncture produced greater short-term results and also produced long-term positive patient outcomes. This indicates that the effective action of true acupuncture is not due to the placebo effect.
Serum serotonin levels increased significantly in the acupuncture and sham acupuncture groups (p<0.001 and p<0.01 respectively), with the increase in the acupuncture group being significantly greater than both sham and simulated acupuncture (p<0.01). Serum Substance P levels significantly decreased in the acupuncture group (p=0.001). There were no significant changes in serum Substance P in the sham group, and there was a significant increase (p=0.001) in the simulated group.
This study suggests that acupuncture is an effective treatment for patients with fibromyalgia, with the ability to improve a wide variety of symptoms, increase serum serotonin levels, and reduce serum Substance P levels. Genuine acupuncture treatment is superior to sham or simulated acupuncture, with improvements in symptoms lasting for several months after completion of all treatments. Contact your local licensed acupuncturist to learn more.
References:
[i] Wolfe F. et al “Serotonin levels, pain threshold, and fibromyalgia symptoms in the general population.” The Journal of Rheumatology [01 Mar 1997, 24(3):555-559].
[ii] Harrison S. Geppetti P. “Substance P” The International Journal of Biochemistry & Cell Biology Volume 33, Issue 6, June 2001, Pages 555-576.