Acupuncture reduces inflammation and researchers have discovered how it works. In a laboratory controlled scientific investigation, a key biological marker has been identified, quantified, and directly correlated with the application of acupuncture. Acupuncture successfully downregulates a proinflammatory biochemical (tumor necrosis factor alpha), which results in anti-inflammatory responses. In addition, the researchers have mapped the neural pathways by which acupuncture signaling stimulates anti-inflammatory effects.
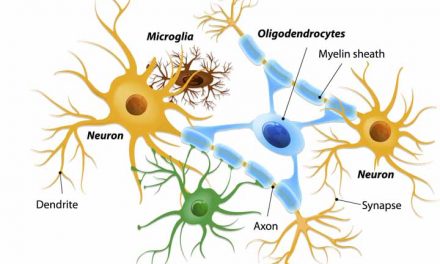
Researchers in Korea have identified a mechanism by which acupuncture stimulation at the acupoint ST36 (Zusanli) has an anti-inflammatory effect. By downregulating tumor necrosis factor alpha (TNF-α), acupuncture relieves systemic inflammation. By testing the effects that a splenic neurectomy and vagotomy have on TNF-α levels in the spleen and the brain, Lim et al. found that the anti-inflammatory effects of ST36 (Zusanli) rely on the vagus nerve pathway. Both manual acupuncture stimulation (MAC) and electroacupuncture (EAC) induce c-Fos protein generation. However, only manual acupuncture stimulation has the effect of downregulating TNF-α; electroacupuncture has the opposite effect when applied to ST36.
Chronic inflammation is involved in a variety of disease processes. Inflammation is part of the body’s natural response to injuries, but if the condition persists it can lead to further damage. There are a number of factors related to chronic inflammation, including TNF-α. As an endogenous pyrogen, TNF-α is primarily involved in the regulation of immune cells. It is able to induce fever, inflammation, apoptosis, inhibit tumor growth, and inhibit virus replication. However, its dysregulation is implicated in the processes of a number of diseases including major depression, cancer, psoriasis, Alzheimer’s disease, and inflammatory bowel disease (IBD). The researchers in this study used lipopolysaccharide (LPS) to induce TNF-α production in lab mice. Next, they performed a real-time polymerase chain reaction (PCR) DNA analysis, which “showed that TNF-α mRNA was highly induced in the spleen following LPS administration and was downregulated by MAC.”
The researchers also gave the mice either a splenic neurectomy or a vagotomy to discern which nerve pathway was responsible for transmitting the anti-inflammatory responses induced by the acupuncture treatments. They found that the TNF-α levels decreased with MAC but were re-elevated in mice with a splenic neurectomy and vagotomy, suggesting that “TNF-α induced in the spleen and the serum after LPS administration may be modulated by AS [acupuncture stimulation].” Another trial showed that CNQX (AMPA receptor blocker) and PPADS (selective purinergic antagonist) — which both inhibit the dorsal vagal complex (DVC) — also decreased splenic TNF-α, which implies the direct involvement of the vagus nerve in the modulation of TNF-α.
The vagus nerve is a cranial nerve best known for innervating the viscera. However, “growing bodies of evidence indicate that vagus nerve activity is important not only for homeostatic regulation of internal organs but also for the regulation of pathologic inflammatory reactions; thus, the vagus nerve acts as a bridge between the neural and immune systems. Notably, VNS can activate the a7 nicotinic acetylcholine receptor on the macrophages in the spleen.”
The cholinergic response, mediated by the vagus nerve, directly controls a proinflammatory response by way of the inflammatory reflex. Several inflammatory diseases are regulated by the ‘cholinergic anti-inflammatory reflex,’ including rheumatoid arthritis, diabetes, and obesity. Additionally, previous research finds that insulin resistance is caused by chronic inflammation resulting from immune and metabolic dysregulation; in addition, a decrease in vagus nerve activity is correlated with obesity. “Selective cholinergic activation within the efferent vagus nerve-mediated arm of the inflammatory reflex can suppress obesity-associated inflammation and reverse metabolic complications. These findings raise the intriguing possibility that dysregulation of vagus nerve-mediated signaling might contribute to the pathogenesis of obesity and its related comorbidities.”
Obesity has reached epidemic levels in many countries and is a precursor for many chronic diseases, including diabetes. Chronic inflammation is “a critical step in the pathogenesis of insulin resistance and type 2 diabetes mellitus. Cholinergic mechanisms within the inflammatory reflex have, in the past 2 years, been implicated in attenuating obesity-related inflammation and metabolic complications. This knowledge has led to the exploration of novel therapeutic approaches in the treatment of obesity-related disorders.”
References
HD Lim et al., “Anti-Inflammatory Effects of Acupuncture Stimulation via the Vagus Nerve,” PloS one. 11, no. 3 (March 19, 2016), accessed February 3, 2017, pp 4-5. ncbi.nlm.nih.gov/pubmed/26991319
Valentin A. Pavlov and Kevin J. Tracey, The Vagus Nerve and the Inflammatory Reflex—linking Immunity and Metabolism, 8, no. 12, accessed February 3, 2017, ncbi.nlm.nih.gov/pmc/articles/PMC4082307/
Yun-Kyoung Yim et al., Electro-Acupuncture at Acupoint ST36 Reduces Inflammation and Regulates Immune Activity in Collagen-Induced Arthritic Mice, 4, no. 1 (August 18, 2006), accessed February 3, 2017, ncbi.nlm.nih.gov/pmc/articles/PMC1810363/
Lin, Lili, Nikola Skakavac, Xiaoyang Lin, Dong Lin, Mia C. Borlongan, Cesar V. Borlongan, and Chuanhai Cao. “Acupuncture-induced analgesia: the role of microglial inhibition.” Cell transplantation 25, no. 4 (2016): 621-628.
Zhang, Ruixin, Lixing Lao, Ke Ren, and Brian M. Berman. “Mechanisms of acupuncture–electroacupuncture on persistent pain.” The Journal of the American Society of Anesthesiologists 120, no. 2 (2014): 482-503.



Recent Comments